English
- HOME
- English
English
Professor's greeting

I am Masatoshi Saito, a professor in the Department of Maternal and Fetal Therapeutics.
This department was established in April 2012 as the "Department of Advanced Interdisciplinary Biomedical Engineering", with my predecessor, Dr. Yoshitaka Kimura, serving as professor. During his time at the Department of Advanced Interdisciplinary Biomedical Engineering, Dr. Kimura and his collaborator focused on developing and successfully commercializing the "fetal electrocardiogram (ECG)," which collects the electrical signals of the fetal heart, the biological information of the fetus in the uterus, from the mother's abdominal wall. Until then, the only real-time fetal biometric information that could be measured was "heart rate variability," and in actual clinical practice, the only way to "estimate" the ever-changing fetal condition was to use this fetal heart rate variability alone. However, the "fetal ECG" developed by Dr. Kimura has made it possible to capture changes in fetal condition at a deeper level and is expected to greatly advance the management of pregnancy and delivery in the future.
After that, I succeeded Dr. Kimura as professor in April 2020, and we are working to take a new step forward as the "Department of Maternal and Fetal Therapeutics".
As mentioned above, the physiological activities of the fetus in the uterus are still a black box. In addition to the mysteries of "development," such as when the fetus senses light and when it hears, we do not know how the experience in the womb affects the baby after birth, whether the environment in the womb is related to the onset of future diseases, what the blood pressure level of the fetus is, what the oxygen saturation level is, and so on.
Our laboratory conducts both basic and clinical research to unravel the mysteries of the intrauterine environment during pregnancy and to create new knowledge and develop completely new diagnostic and therapeutic methods.
We will continue to make advancements in order to protect the health of mothers who are about to give birth, and the health of babies who are about to be born, through the power of "Maternal and Fetal Therapeutics".
Introduction of Prof. Saito's research

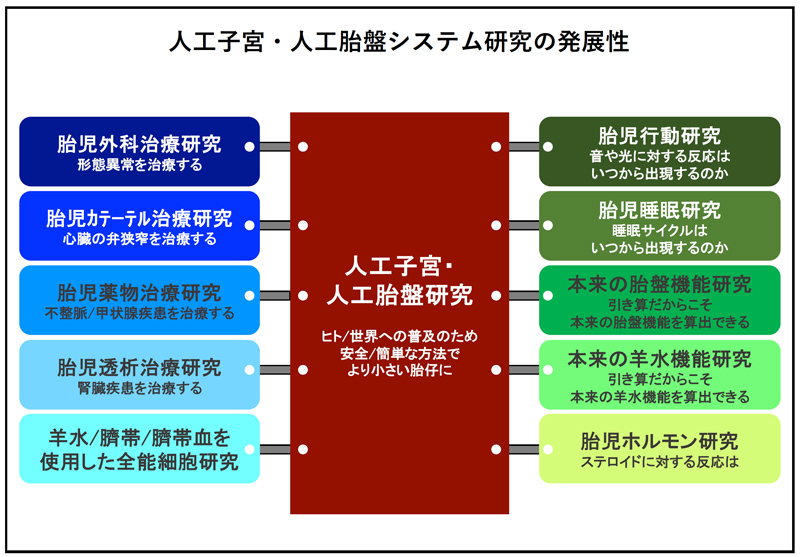
The main theme of my research will be research on artificial uterus and artificial placenta systems.
Japan's performance in perinatal care is among the best in the world, but the rate of preterm birth is said to remain high at about 5-6%. In addition, this trend is expected to continue in the future due to the aging of the population, and preterm birth is a major problem.
In addition, in current neonatal treatment, the limit of treatment is said to be around 22-23 weeks of gestation, the so-called "growth/development limit," which is thought to be due to the immaturity of lung function, circulatory function, and immune function, including skin maturation. We know that it is best for the unborn baby to continue growing in the mother's womb, but for various reasons on both the mother's and the fetus' side, the fetus will get sicker and sicker in the womb, or worse, die, unless the policy is changed from premature birth to neonatal care, such situations are not uncommon in comprehensive perinatal centers. In order to obtain basic data to improve the survival rate of these "growth/development limited" babies, we began research on the "artificial uterus/placenta system" using pregnant sheep.
At the beginning of the experiment, it was difficult to obtain data due to the decrease in circulating blood volume caused by extreme desiccation and heart failure caused by the load of the artificial placental circulation, and so on. However, by introducing artificial amniotic fluid, parallelizing the artificial placental circuit, improving the material and hardness of the artificial umbilical cord, etc., we have now been able to achieve about 2 weeks of survival. We are currently collecting baseline data on this artificial placenta/uterus system so that it can be more safely attached to even smaller babies.
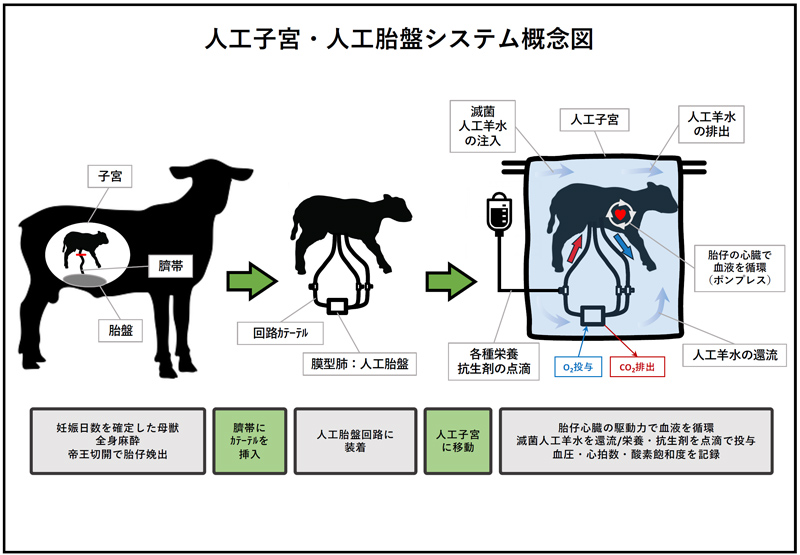
Another feature of this artificial placenta/uterus system is its ability to provide direct access to the fetus while simulating the intrauterine environment of the mother. In other words, it is possible to treat congenital morphological anomalies directly on the patient's fetus. At present, it is common for fetuses with congenital morphological abnormalities to continue their pregnancies in order to "mature and grow as much as possible" in view of the possibility of treatment. However, during the gestational period of maturation and growth, the congenitally dysmorphic fetus may deteriorate irreversibly, or functional problems may occur due to the dysmorphic fetus, making optimal post-delivery treatment impossible. To address these dilemmas, we are investigating the possibility of fetal surgery and fetal catheterization on an artificial placenta/uterus system.
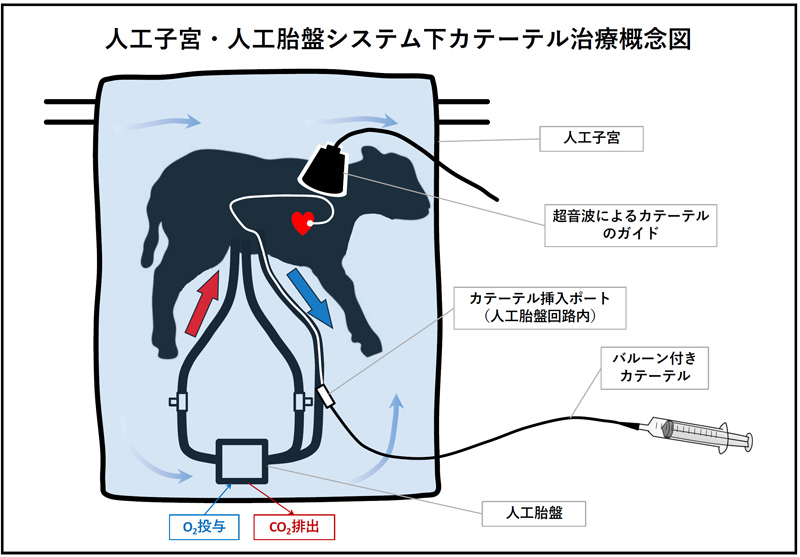
The artificial placenta/uterus system platform can be used for medical treatment and developmental research of fetal biological functions other than those mentioned above. The "maternal, placental, umbilical cord and amniotic fluid knockout model" has the potential to be used for the analysis of these original functions and functions yet to be elucidated by subtraction.
Prof. Saito's Research AchievementsLink to Researchmap
- Saito M, Matsuda T, Okuyama K, Kobayashi Y, Kitanishi R, Hanita T, Okamura K. Effect of intrauterine inflammation on fetal cerebral hemodynamics and white-matter injury in chronically instrumented fetal sheep. American Journal of Obstetrics & Gynecology. 2009 Jun;200(6):663.e1-11.
- Kemp MW, Saito M, Newnham JP, Nitsos I, Okamura K, Kallapur SG. Preterm birth, infection, and inflammation advances from the study of animal models. Reproductive Sciences. 2010 Jul;17(7):619-28.
- Saito M, Payne MS, Miura Y, Ireland DJ, Stock S, Kallapur SG, Kannan PS, Newnham JP, Kramer BW, Jobe AH, Keelan JA, Kemp MW. Polymyxin B agonist capture therapy for intrauterine inflammation: proof-of-principle in a fetal ovine model. Reproductive Sciences. 2014 May;21(5):623-31.
- Kumagai Y, Kemp MW, Usuda H, Takahashi T, Takahashi Y, Hamada H, Schmidt AF, Hanita T, Watanabe S, Sato S, Ikeda H, Fee EL, Furfaro L, Newnham JP, Jobe AH, Yaegashi N, Saito M. A Reduction in Antenatal Steroid Dose Was Associated with Reduced Cardiac Dysfunction in a Sheep Model of Pregnancy. Reproductive Sciences. 2023 Nov;30(11):3222-3234.
- Usuda H, Ikeda H, Watanabe S, Sato S, Fee EL, Carter SWD, Kumagai Y, Saito Y, Takahashi T, Takahashi Y, Kawamura S, Hanita T, Saito M, Kikuchi A, Choolani MA, Yaegashi N, Kemp MW. Artificial placenta support of extremely preterm ovine fetuses at the border of viability for up to 336 hours with maintenance of systemic circulation but reduced somatic and organ growth. Frontiers in Physiology. 2023 Aug 24;14:1219185.
Introduction of Prof. Kimura's research
Preterm births (deliveries between 22 and 36 weeks of gestation), in which babies are born before full term, are on the rise worldwide. Saving preterm babies is one of the most important issues in perinatal care in an aging society with a low birth rate. In addition, the hospital and family incur significant medical costs for each preterm infant admitted to a neonatal intensive care unit (NICU) before discharge. Surprisingly, however, there is still no reliable management and treatment of preterm birth, and there is no uniformity around the world.
Currently, heart rate monitoring, one of the fetal condition assessments, is performed using an ultrasound Doppler device. In this method, the heart rate is calculated from the fetal heartbeat using ultrasound, which is a problem in the second trimester of pregnancy because it is difficult to keep the ultrasound focused on the small fetal heart. In the third trimester, stable fetal heart rate monitoring is possible, but detailed changes in heart rate have not been recorded (see Figure 1).
Therefore, in collaboration with a company (*1), we have developed and successfully marketed a fetal heart rate monitor, Iris Monitor®, based on a completely new principle of extracting tiny fetal bioelectrical signals from mixed maternal and fetal bioelectrical signals obtained from the mother's abdominal wall (approved by the Ministry of Pharmaceutical Affairs on February 23, 2009). The device has been proven in clinical trials from 24 weeks of gestation and is the world's first device to non-invasively measure fetal heart rate from this stage through the maternal abdominal wall. With the rise in preterm births, the need for fetal heart rate monitoring in the second trimester is increasing and the addition of the Iris Monitor® to existing products is expected to improve the accuracy of fetal monitoring.
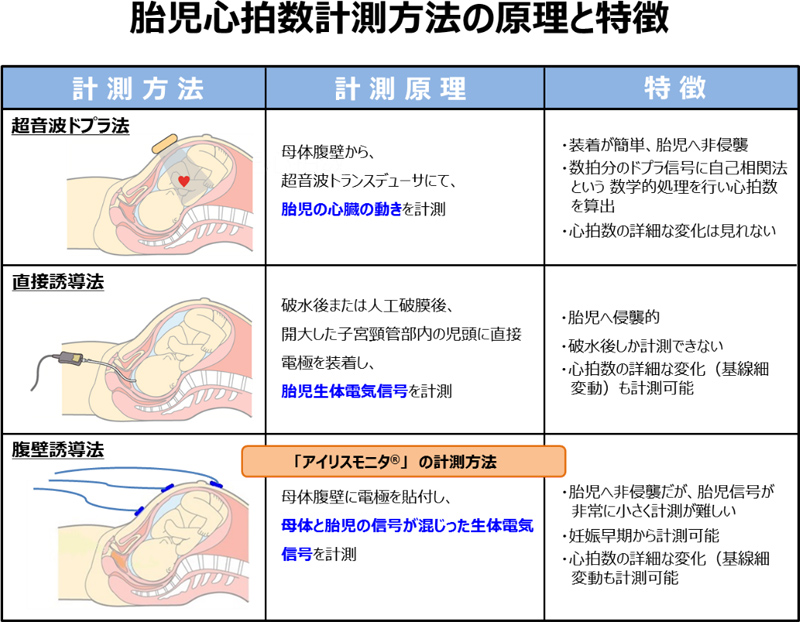
Figure 1: Principles and characteristics of fetal heart rate measurement methods
The actual fetal ECG is measured by placing several electrodes on the mother's abdomen. The signal obtained from the mother's abdomen includes the mother's electrocardiogram, electromyogram, and environmental noise in addition to the fetal electrocardiogram. The amplitude of the fetal ECG is about 5 μV to 20 μV, the mother's ECG is about 1000 μV, and the EMG is about 100 μV. We developed the reference system independent component analysis method (*2) as a new information theory to extract only the fetal ECG from the mixed signals. (see Figure 2).
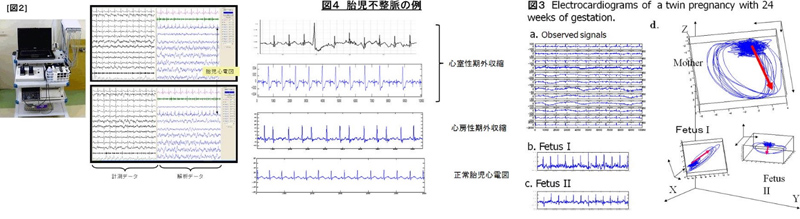
Figure 2: New information theory for extracting fetal electrocardiograms.
As the second new information theory, we are developing reference-based AI (*3) that overcomes the disadvantages of AI used in machine learning, which is currently being actively introduced in various fields (i.e., the need for a large amount of teacher data and the difficulty of verifying why the results obtained are the way they are). This technology is capable of deriving highly accurate results through self-learning based on a small amount of teacher data, and is characterized by the verifiability of the judgment process. (See Figure 3).

Figure 3. Information Theory of New Machine Learning
As mentioned above, there are still many things in the field of obstetrics, including preterm birth, that are not fully understood. We will continue to take on the challenge of solving these problems using new information theory, which is one of our strengths.
*1.Collaborative Research Company: Atom Medical Corporation
*2.Japanese Patent No.4590554
*3.Japanese Patent No.7330521
Dr. Kimura is a board member of a Tohoku University venture company that uses the aforementioned patented technology.
Prof. Kimura's Research AchievementsLink to Researchmap
- Kimura Y, Okamura K, Watanabe T, Murotsuki J, Suzuki T, Yano M, Yajima A. Power spectral analysis for autonomic influences in heart rate and blood pressure variability in fetal lambs. American Journal of Physiology - Heart and Circulatory Physiology, 271(4): H1333-9 (1996)
- Kimura Y, Okamura K, Watanabe T, Yaegashi N, Uehara S, Yajima A. Time-frequency analysis of fetal heartbeat fluction using wavelet transform. American Journal of Physiology- Heart and Circulatory Physiology, 275(6): H1993-9 (Dec 1998)
- Sato M, Kimura Y, Chida S, Ito T, Katayama N, Okamura K, Nakao M. A Novel Extraction Method of Fetal Electrocardiogram From the Composite Abdominal Signal. IEEE Transactions on Biomedical Engineering, 54(1): 49-58 (Jan 2007).
- Sato N, Hoshiai T, Ito T, Ohwada K, Chisaka H, Aoyagi A, Sugawara J, Yaegashi N, Okamura K, Kimura Y. Successful Detection of the Fetal Electrocardiogram Waveform Changes during Various States of Singletons. The Tohoku Joumal of Experimental Medicine, 225(2): 89-94 (2011/Sep. 09, 2011)
- Oshio S, Kimura Y, Nishigori H, Sato N, Minato T, Khandoker AH, Owada K, Sudo K, Odagiri N, Yaegashi N. A Comparison Study on Safety and Efficacy of Maternal Abdominal-Lead Fetal ECG Under Regulatory Science. Advances in Clinical and Translational Research, 2(2): 1-12 (Jul 2018)
Introduction of Dr. Kasahara's research

The time that a baby spends in its mother's womb is crucial for the development of its body. During this period, various events that are transmitted from the mother can affect the baby's future health and susceptibility to disease. The term DOHaD stands for Developmental Origin of Health and Disease. It refers to the idea that environmental factors during the embryonic, fetal, and early postnatal periods can impact future health and disease risk. A child's future health and risk of disease are determined by genetic and environmental factors, either acting alone or in combination. These factors are believed to play a significant role in determining a child's health and susceptibility to disease. DOHaD focuses on how environmental factors during the embryonic, fetal, and early postnatal periods affect the child's future health. Previous studies in humans and mice have shown that infants with low birthweight due to maternal undernutrition during pregnancy are at increased risk of developing obesity and diabetes in the future. Additionally, maternal infections during pregnancy increase the risk of future neurodevelopmental disorders and schizophrenia in the offspring.
Based on the concept of DOHaD, our research group focuses on neurodevelopmental disorders, such as autism spectrum disorder (ASD), and metabolic disorders, such as diabetes, caused by environmental factors during fetal development. We conduct research using mice to determine the biological changes and mechanisms that lead to the onset of these diseases due to environmental influences during fetal life.
Neurodevelopmental disorders, such as ASD, and metabolic diseases, such as diabetes, cause an imbalance between sympathetic and parasympathetic nerves, resulting in abnormal autonomic nervous system function. Our research group believes that abnormal autonomic nervous system function occurs as a biological change due to environmental factors during the fetal period. This change may act as a vulnerability over a long period of time and lead to the risk of developing diseases in the future. We are studying when and how the autonomic nervous system functions change (see Figure).
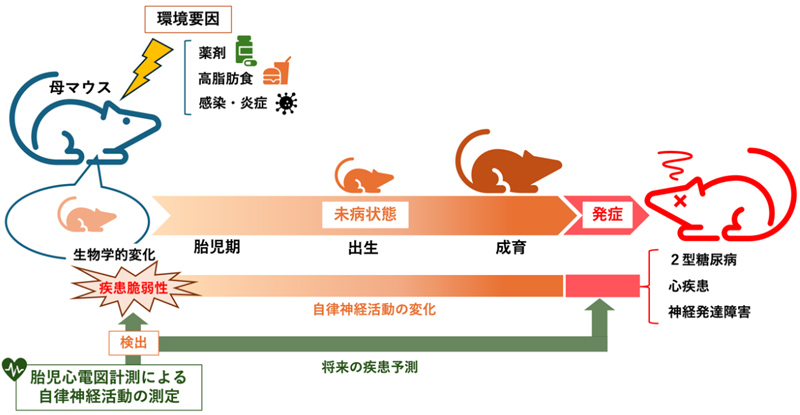
Autonomic activity can be assessed from heart rate variability. It is well known that heart rate can be faster or slower under the influence of sympathetic and parasympathetic nerves. It is therefore possible to infer sympathetic and parasympathetic activity from heart rate variability. Until now, it has been difficult to accurately measure the heart rate of mouse fetuses, but we have developed a technique in our laboratory that allows us to measure the electrocardiogram of mouse fetuses with high accuracy over a continuous, long period of time. We use this technology to measure fetal electrocardiograms from mouse models of neurodevelopmental disorders and diabetes mellitus to assess autonomic nervous system activity. In addition, the "human fetal electrocardiogram device" developed by Dr Yoshitaka Kimura in our laboratory can measure the electrocardiogram of human fetuses. Since the same indicators can be used for evaluation in humans and mice, we believe that the results of research in mice will provide important knowledge directly related to clinical practice in humans, leading to very early diagnosis and very early treatment of diseases from the fetal stage.
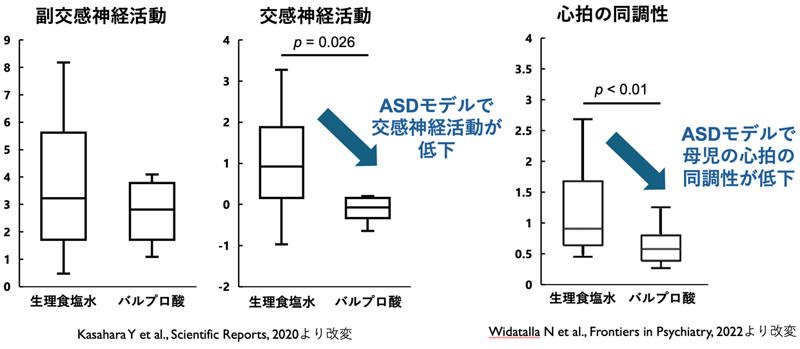
Our research group has previously measured the electrocardiogram of mouse fetuses and assessed autonomic nervous system activity using a fetal valproic acid administration model, which is one of the ASD model mice. We found that sympathetic nervous system activity is reduced in the fetuses of ASD model mice (Kasahara Y et al., Scientific Reports, 2020). The dysregulation of the autonomic nervous system continued after birth, confirming that the pups showed impaired social behaviour as adults. The ASD model mice also showed reduced synchrony between maternal and fetal heart rate variability (Widatalla N et al., Frontiers in Psychiatry, 2022). Reduced synchrony of heart rate variability with the mother, the only other person for the fetus, may be a "communication disorder with others" in a broad sense, suggesting that this may be one of the as yet undiscovered symptoms of ASD.
We are also conducting fetal autonomic evaluation using mouse models of maternal inflammation, aging, and diabetes, with some very interesting results. In addition, we are conducting an integrative study of diseases caused by DOHaD by combining behavioral tests to assess social skills, anxiety, and depression, gene expression analysis, and histological analysis.
Dr. Kasahara's Research AchievementsLink to Researchmap
- Widatalla N, Khandoker AH, Yoshida C, Nakanishi K, Fukase M, Suzuki A, Saito M, Kimura Y, Kasahara Y. Correlation between maternal and fetal heart rate increases with fetal mouse age in typical development and is disturbed in autism mouse model treated with valproic acid. Frontiers in Psychiatry, 13: 998695 (2022) doi: 10.3389/fpsyt.2022.998695
- Kasahara Y*, Yoshida C*, Saito M, Kimura Y (*; co-first). Assessment of heart rate and sympathetic and parasympathetic nervous activities of normal mouse fetuses at different stages of fetal development using fetal electrocardiography. Frontiers in Physiology 12: 482 (2021) doi: 10.3389/fphys.2021.652828
- Kasahara Y, Yoshida C, Nakanishi K, Fukase M, Suzuki A, Kimura Y. Alterations in the autonomic nerve activities of prenatal autism model mice treated with valproic acid at different developmental stages. Scientific Reports 10: 17722 (2020) doi: 10.1038/s41598-020-74662-0
- Kasahara Y, Sakakibara Y, Hiratsuka T, Moriya Y, Lesch KP, Hall FS, Uhl GR, Sora I. Repeated methamphetamine treatment increases spine density in the nucleus accumbens of serotonin transporter knockout mice. Neuropsychopharmacology Reports 39(2): 130-133 (2019)
- Kasahara Y, Sato K, Takayanagi Y, Mizukami H, Ozawa K, Hidema S, So KH, Kawada T, Inoue N, Ikeda I, Roh SG, Itoi K, Nishimori K. Oxytocin receptor in the hypothalamus is sufficient to rescue normal thermoregulatory function in male oxytocin receptor knockout mice. Endocrinology 154(11): 4305-4315 (2013)
- Takayanagi Y*, Kasahara Y*, Onaka T, Takahashi N, Kawada T, Nishimori K (*; co-first). Oxytocin receptor-deficient mice developed late-onset obesity. Neuroreport 19(9): 951-955 (2008)